Hey everyone!
I’ve been thinking a lot recently about different ways to classify different types of SI joint dysfunction and pain.
When most people think of SI joint dysfunction, they think of it as the result of a musculoskeletal injury. However, there are other potential reasons for why people may experience SI joint pain.
Sometimes, you can have an underlying medical condition that’s actually causing your SI joint pain, or makes you more sensitive to having any kind of an injury.
If you have something like this going on, it can be so important to figure out, so you can find the right specific treatments.
In this post, I’m going to describe four main types of SI joint issues.
As you read through the list, you may find that more that one category applies to you. And that’s totally fine– I myself would have fallen into the the first three categories, at different points during the time period I’ve written about on my blog.
However, I feel this is the best framework to help you understand the different potential reasons for how your SI joint issues started, and which factors may be contributing to them now.
So, the types….
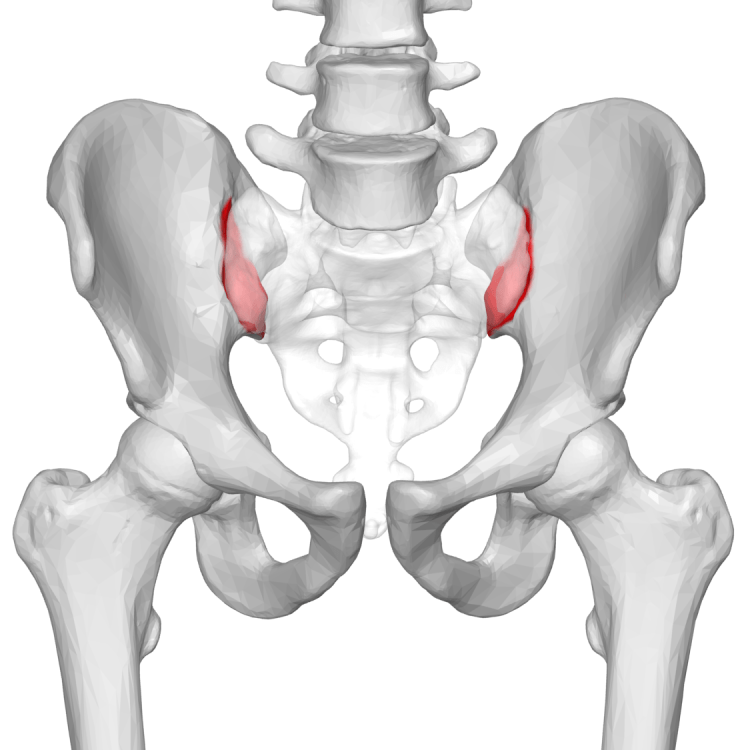
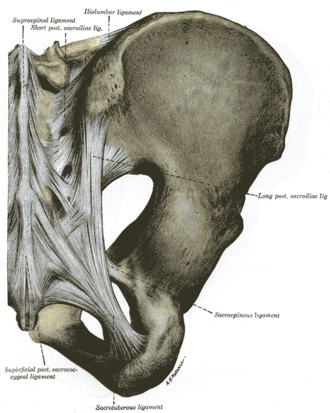
Type 1: Joint Hypermobility due to a Ligament Injury
Joint hypermobility means that a joint is moving more than it should, in this case because the ligaments are stretched out.
My friend Kelsey struggled with SI joint dysfunction for a few months, at one point in time, however her case was pretty easily resolved compared to mine.
She had stretched out the ligaments in her right SI joint because she was in a car accident where she was rear-ended, while she was stomping her foot down on the break. That impact created too much force for her SI joint ligaments, so it created a lot of pain.
However, Kelsey was able to recover with one course of physical therapy, with the first physical therapist she happened to see. (God, could we all be that lucky!).
Her pain was caused by her right SI joint moving beyond its normal range of motion. Any time you have a joint that’s moving too much, it puts strain on all of the ligaments of the joint (not just the one that may have been initially injured). It also overworks the muscles, which can spasm up to protect the area, and create inflammation.
This, obviously, can be painful.
However, Kelsey never seemed to experience the main symptom that has plagued me, which is my joints moving out of place and staying that way.
Type 2: Hypermobility can lead to hypomobility: Joints that get stuck in an abnormal position
Here’s the thing about hypermobile SI joints. In some people (like me), the hip bones can rotate out of place, in relation to the base of the spine, and then stay that way.
With my SI joint dysfunction, my worst symptom actually wasn’t the pain. It was that one of my SI joints would get “stuck,” and I wouldn’t be able to fully use the leg on that side. Then that would create pain, but it seemed to be more as a result of having my leg restricted. If I didn’t move, it usually didn’t hurt.
So in technical terms, you have a joint that was hypermobile (moving too much). However, now that one of the hip bones has moved so far that it’s jammed against the base of the spine, it has become hypomobile.
Why does this happen?
For one thing, I believe it can have a lot to do with the nature of your injury. Exactly which ligament(s) did you sprain? How strong were your muscles prior to the injury?
Another factor is the make-up of your individual joints. In my physical therapy prerequisite classes, I’ve learned that there are multiple factors that can affect how stable a joint is, based on its shape. Some people are simply born with more stable joint shapes than others.
As you’ll see in my next point, some people also have ligaments that are not quite as sturdy as others, which can also be a factor in how far their SI joints can move.
Type 3: Joint Hypermobility that’s genetic
For much of my life, I didn’t know that I had a genetic hypermobility condition. It’s something I’ve only really come to understand in my 30’s.
Now I know that my body produces connective tissue differently than a “normal” person. As a result, my ligaments, tendons, and other connective tissues a little bit “stretchier” than they’re supposed to be.
In general, if you’re genetically hypermobile, it is going to unfortunately be easier for you to develop injuries that involve a ligament sprain and/or altered joint mechanics… such as SI joint dysfunction. So I do believe a higher percentage of my readers are likely to be hypermobile, as compared to the average population.
To be clear, there are a range of connective tissue disorders that can have different symptoms, depending on which types of proteins are affected. A geneticist can help to evaluate and narrow things down further.
However, as a general overview, here are some of the symptoms to look out for:
- Flat feet
- “Double-jointed”– people with connective tissue disorders are likely to have been those kids growing up who could do all kinds of crazy tricks bending their fingers and hands
- Chronic, widespread pain
- A history of joint dislocations (shoulder, hip, etc).
- Frequent injuries, such as ankle sprains
There are other symptoms which may also be part of hypermobility disorders, such as fatigue, light-headedness, and digestive issues, to name a few.
This is why it’s so important to check in with a medical professional. If you think you may have a genetic hypermobility condition, you can consult a geneticist for further information.
Type 4: An Inflammatory Condition due to a Genetic Condition or Illness
If you’ve heard the term “sacroillitis,” it most directly applies to this category, as it means “inflammation of the SI joint.”
This category is somewhat distinct from the other three, because the main cause does not necessarily start with the ligaments, but deeper within the joint itself.
Why can the SI joint become inflamed?
Some people develop inflammation in the SI joint due to an infection. This may be more likely to occur if you’ve had surgery recently.
Another reason is that you may have an autoimmune condition that causes inflammation within the SI joints. For example, a condition known as anklyosing spondylitis can first appear as pain within the SI joints. The inflammation of AS can also cause the joints to fuse together– limiting their motion and creating hypomobility. (Remember, hypomobility means “not moving enough,” so it is the same term even though the cause may be different from Type 2, above).
There are other autoimmune conditions which can cause pain within the SI joints, as well. Some of these conditions include lupus, psoriatic arthritis, and rheumatoid arthritis. If you’re concerned that you may have an autoimmune condition, I recommend consulting a rheumatologist. This is a well-written article that explains further.
People with mast cell activation syndrome can also experience inflammation– not only in the SI joints, but in other locations within the body as well.
Please know that if have any of these conditions, there is hope!
So, these are my main four.
I hope this post is not too doom-and-gloom! I know that many of you are looking for this information, so this post is my best effort to help clarify.
Yet, please know that there are treatments available for every single condition that I just mentioned!
It just comes down to being persistent, and finding the right medical professionals to treat you.
So… what do you guys think?
What has your experience been like trying to get a diagnosis? Which category do you feel you fit into?
Feel free to chime in below!
I’m honored that you linked to my blog! 😀 It’s nice to have an organized list of all the causes of joint hypermobility. I never thought of becoming hypermobile from an injury, but I knew people who probably were hypermobile from their bone structure when I was taking ballet lessons. I wonder what effect sports that encourage flexibility have on joints in the long-term. Do people get hypermobile joints simply from all the stretching in ballet, even if their bone structure doesn’t make them hypermobile? Or is it really just that they are flexible, but they don’t have joint hypermobility?
LikeLike
Of course! I love your blog!
Hmm… I’ve thought a lot about your question! I don’t know much about ballet, but I found this article on how SI joint injuries can actually be a pretty common result of yoga poses that stretch out the ligaments: https://www.yogajournal.com/yoga-101/anatomy-101-understanding-sacroiliac-joint
I think the takeaway from this is that any activity that stretches out the ligaments and creates extra mobility in the joint is likely to result in pain and injury. Our ligaments are supposed to be a certain length, and any “wiggle room” beyond that, so to speak, does not help us. So, if someone is able to keep up with the rigorous demands of ballet dance, I would guess that the main factor is that they have more muscle flexibility than the average person, and possibly some hypermobility due to bone shape (which doesn’t necessarily lead to injury right away, just makes you prone to injury).
Hope that makes sense!
LikeLiked by 1 person
Yes, that makes sense! When I was taking ballet lessons in middle school there was a lot of emphasis on strengthening so we could handle the flexibility, and on being careful not to overstretch. For the first three years, we did strengthening exercises on the floor at the beginning of every class.
LikeLiked by 1 person
Hi
I found your blog this morning. Have been suffering with pain, sometimes extreme and debilitating, for almost 3 years. It is extreme in the later part of the day if I have been on my feet for any length of time. I recently skyped with a Dr. of PT who diagnosed SI issues. I am doing a series of exercises, which he believes with help within 3-5 weeks. It is so hard to be patient and trust I am on the right path after many wrong diagnosis… bulging disc, compromised nerve etc.
Thanks for your encouragement and hope that I will eventually get some relief.
Dawn
LikeLike
Hi Dawn, I’m happy to help! Yes, this condition definitely can get better! It sounds as though you’re on the right track, now that you have a diagnosis and someone to treat you. Sometimes there can be process of trial and error that you have to go through to find what works, because what works for one person may not work for another. But with persistence you can absolutely find a path forward!
LikeLike
I haven’t incurred any injuries but I have SI Joint disfunction and am considered to have sacroiliitis. I do however have celiac disease and when I consume gluten, my joints become inflamed. My doctor thinks this may be an extreme case of an inflammatory responce to gluten. Just a thought!
LikeLike
Hi Sheri, so sorry to hear you’re dealing with this, but that certainly is an interesting theory. I think it’s definitely possible. (This would put you into Type 4: Inflammatory).
I can actually really relate to this because of the stabbing joint pain I once had during my worst flare up of mast cell activation syndrome.
It is pretty crazy how the immune system can cause such extreme joint pain.
Wishing you the best of luck on your healing journey!
LikeLike